The Estrogen-Cancer Myth: How Hormone Deficiency Leaves Women Vulnerable

"Estrogen causes cancer", is what many took away from the Women's Health Initiative (WHI). But do we really know that, or have we just been told that?
The fear of hormone replacement therapy (HRT), like the Sword of Damocles, looms over the heads of all who dare use or prescribe estrogen replacement therapy. The frequent negative media reports on breast cancer, as well as Black Box warnings, preclude women from feeling safe to take it, and doctors reluctant to prescribe it.
Let's Take a Closer Look
The fear of breast cancer, coupled with the general condemnation of the use of HRT by physicians, poses an insurmountable obstacle to millions of women gaining access to the treatments they need. Following the release of the unsettling results of the WHI study, millions of women abruptly stopped taking their HRT at the advice of their physicians and on their own. Prior to 2002, Premarin was the #1 prescription drug sold in the world. Now it is the most likely drug to be discontinued and the least likely drug to be prescribed.
Proponents of the WHI, The Million Women’s Study, and data from numerous other studies and cancer registries argue that the data are irrefutable. HRT is associated with a significant increase in the incidence of breast cancer. They are right if you consider the use of drugs that have hormone-like effects used in these studies the same as rhythmic bioidentical hormone restoration therapy (BHRT). No one seems to talk about this important difference. Yet the indictment is of all formulations of HRT without discrimination.
Physicians perplexed by the unexpected results of the Women’s Health Initiative were forced to reevaluate the study. As a result, many questions about the validity of the findings and the soundness of the study were raised. What insight emerged from the WHI study is that the use of synthetic estrogen and progestin replacement remains questionable at best.
Numerous experts and research scientists disagree with the conclusions promoted by the WHI, but unfortunately, these conclusions remain the current standard from which medical society position papers, FDA Black Box warnings, and therapeutic recommendations are currently derived. Dr. Steven Goldstein, professor of obstetrics and gynecology at New York University, stated that extrapolation from the Women’s Health Initiative (WHI) to other forms of hormone replacement therapy is unfair and inappropriate. The broad interpretation and publicity as a result of the WHI resulted in a general condemnation of all HRT in postmenopausal women. In fact, a careful review of the extensive literature suggests that data resulting from the WHI and other recent studies should only be interpreted within the narrow context of the study design.
Dr. Leon Speroff, professor of obstetrics and gynecology, and reproductive endocrinology at Oregon Health Science University, Portland, and author of the textbook, Clinical Gynecologic Endocrinology and Fertility, said in an interview, “The initial negative impact of the Women’s Health Initiative is over, we know the study's limitations, we know that some of the conclusions promoted in the medial were not correct, and we know that the risks that have been promoted by the Women’s Health Initiative are incredibly small and perhaps not real.”
Something to consider when taking estrogen is that not all estrogens are created equal. Estradiol, the principal estrogen in women, interacts through its receptors with thousands of distinct target genes in the nucleus of cells, with the ability to precisely discriminate function across different cell types. The specific message estrogen communicates varies with precise changes in the timing of delivery and the amount of estrogen found in the blood. In the young, healthy reproductive female, estrogen is delivered into the blood from the ovaries in a wave-like rhythmic pattern over her 28-day menstrual cycle, interacting with her brain, uterus, and all other tissues and organs of her body. Day one of the menstrual cycle begins with low levels of estrogen, quiet like a distant drum roll that builds and grows until the crescendo rise in estrogen levels heralds the advent of a ripe egg. New life is the timeless theme of estrogen, while at the same time assuring the preservation of existing life. Depending on the specific cellular response, estrogen regulates all growth, healing, and repair functions throughout a woman's body, assuring her life.
For this reason, the substitution of a synthetically modified estrogen or the estrogen from another species will not replicate the desired results throughout her system and can throw a woman’s physiology out of balance, causing a cascade of mental and physical malfunction. Currently, the primary estrogen being used clinically and in randomized clinical trials is an equine estrogen, known as Premarin (pregnant-mare-urine). Pregnant mares are catheterized, and the hormones are extracted from their urine.
If a critical amount of estrogen is in fact essential for normal female development, shape, tone, and function of the breast, then logic would dictate that a critical amount of estrogen is essential in maintaining the health of the breast. It is only after estrogen levels begin to decline, when women enter their thirties, do we see the appearance of breast pathologies such as breast pain, fibro-adenomatous, and fibrocystic changes. Excluding certain genetic mutations (such as BRACA-1 and BRACA-2), it is only when estrogen becomes deficient do we also see a progressive rise in the rate of breast cancer.
Estrogen deficiency, not high estrogen, remains the greatest risk factor for developing breast cancer.
At age 25 a woman has a 1 in 19,608 risk of developing breast cancer. By age 30, that risk is increased to 1 out of 2,212, by age 50, that risk is increased to 1 out of 54, and by age 85, that risk is increased to 1 out of 9. A female born today, assuming current rates stay constant, has a 1 in 8 chance of developing breast cancer during the course of her life. What differentiates a 25-year-old female from a 35 or 55-year-old female is the declining egg count that reduces her capacity to produce adequate amounts of estrogen. It is therefore insufficient estrogen levels associated with the aging process that actually place the aging female at a higher risk of breast cancer.
The length of time a woman has been estrogen-deficient is a stronger predictor of breast cancer. The longer a woman remains in a state of estrogen deficiency, the more likely she is to develop breast cancer.
Nearly 70 percent of the participants in the Women’s Health Initiative were between the ages of 60 and 79. Most of them had been in a state of estrogen deficiency for decades. It takes a breast cancer cell 10-20 years to become clinically detectable. Since most of the cancers were discovered early in the study, one could correctly conclude that the majority of the women in the study who developed breast cancer had previously undiagnosed breast cancer at the time they entered the study. The hormones simply uncovered the breast cancer. Not a single study to this date has found an increase in hormone users in the earliest stage of breast cancer (noninvasive, in situ disease). In light of this data, to conclude that hormone replacement therapy is causal to breast cancer defies logic. The Women’s Health Initiative is more of a study of the impact of aging on a woman’s body rather than the impact of hormone replacement therapy.
Contrary to popular belief, there is a growing body of evidence in the scientific literature that sufficient estrogen is essential for breast health and the reduced risk of breast cancer. Not only does estrogen have a primary breast cancer prevention function, but a secondary breast cancer prevention function through its promotion of the production of progesterone.
It is understandable how the notion came to be accepted that estradiol plays a role in breast carcinogenesis. Estrogen’s functions are mediated by multiple mechanisms, both genomic through its receptors, and multiple non-genomic (ER-independent) interactions. Low levels of estradiol induce powerful signals for cell growth (G1 activation). Estrogen levels can be low for 10 to 15 years prior to the climacteric, accounting for the development of PMS, PMDD, and anovulatory menstrual cycles, mostly depicted as painful, heavy, and debilitating. It should be noted that the rise in breast cancer rates corresponds exactly to that time in a woman’s life when her estrogen levels begin to decline. Once a woman transitions into post menopause, her estradiol levels remain relatively low, also resulting in a stronger signal of the proliferation of breast tissue. Conventional hormone replacement practices result in relatively low estrogen, which may account for the rise in breast cancer observed in many studies.
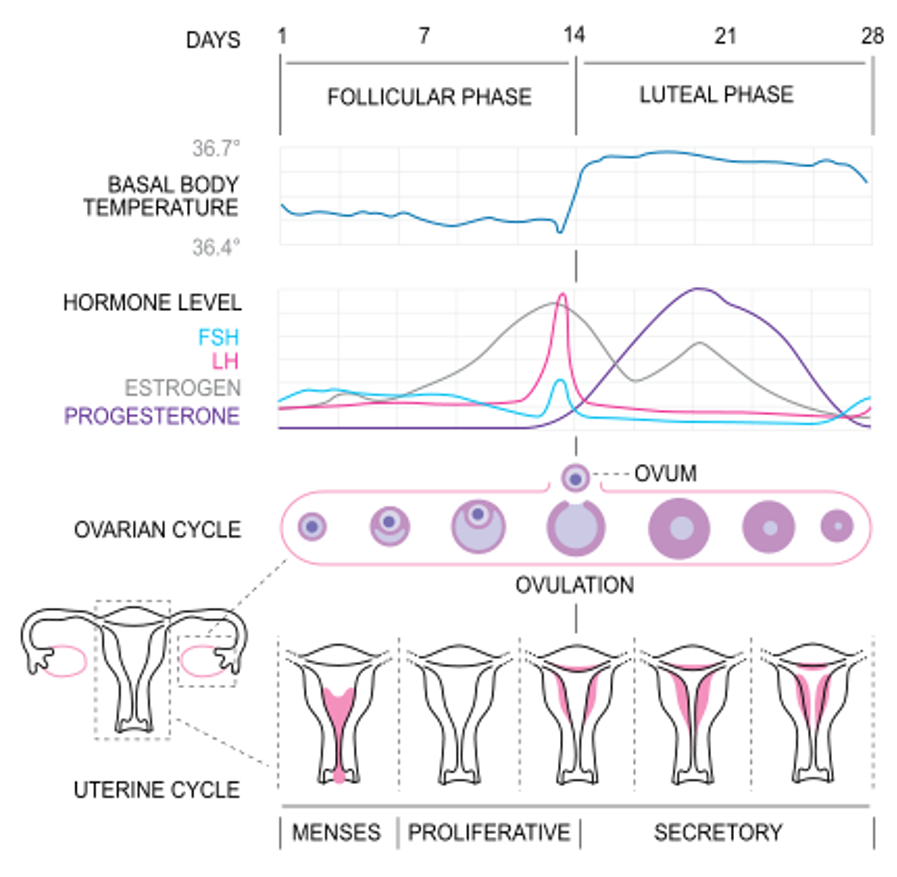
During the initial phase of a normal menstrual cycle, estrogen levels are low, resulting in the growth of the endometrium and breast tissue. Just prior to ovulation, estradiol levels rise in a gradual and steady spike, altering the genomic instructions to signal cellular growth inhibition (G1 arrest), induction of apoptosis (programmed cell death), and promotion of ovulation.
“Interestingly, at high concentrations, estradiol inhibits proliferation and induces apoptosis.” Apoptosis is required for normal development and tissue homeostasis. The loss of regulation of apoptosis is fundamental to the development of diseases, such as cancer, stroke, heart disease, neurodegenerative disorders, and autoimmune disorders. “Ironically, high doses of estrogen can induce regression of hormone-dependent breast cancer in postmenopausal women. Laboratory studies show that the apoptotic action of estrogen is the major factor leading to cell number decreases in several cell types. The effects of estrogen are estrogen-receptor dependent.”
“A team of researchers at CIC bioGUNE has revealed that estrogen can reduce the risk of breast cancer. Their work shows that estrogen is capable of reducing the number of breast cancer stem cells, which may explain the lower progression of the tumor and, as a consequence, the possibility of a better prognosis. However, nothing or little has been known until now about the effect of estrogen on the tumor-initiating cells.” Marie Vivanco, leader of the research team, believes that this study represents a new functional aspect of estrogen due to its capacity to act in a different way depending on the cellular type.
The evidence in favor of estrogen therapy reducing a woman’s risk of breast cancer can be found in the estrogen-progestin arm of the WHI. Patients who adhered to treatment throughout the study had a significant reduction in the risk of breast cancer. In the estrogen-only arm of the WHI, women who adhered to treatment throughout the study had a 33 percent reduction in the risk of breast cancer. In a study published in the Journal of the National Cancer Institute, women who received estrogen-only therapy for between 10–15 years conferred a 7 percent reduction in the risk of breast cancer. In a study performed at MD Anderson on 309 women with localized breast cancer, there was a significant reduction in the recurrence of breast cancer in the estrogen group.
Historically, HRT is typically avoided for women with a history of breast cancer because of concerns that estrogen will stimulate recurrence. A survey on breast cancer survivors in menopause found that women were more concerned about the risk of breast cancer recurrence than about the risks of osteoporosis and heart disease. Yet breast cancer survivors are interested in treatments that may improve the quality of their lives. There is a growing body of new evidence that the use of hormone replacement therapy is associated with a low probability of detrimental effects in early-stage breast cancer survivors. Several studies observed lower risks of recurrence and mortality in women who have used HRT after their breast cancer diagnosis than in women who did not.
Numerous studies are discussing potential implications for the treatment and control of breast cancer with high-dose estrogen as a specific therapeutic agent in postmenopausal women using estrogen-mediated processes. Estrogen and progesterone (whose production and receptor expression is estrogen-dependent) play a critical role in controlling steroid-mediated cellular growth regulation in female biology. It is the loss of normal growth control that is the hallmark of cancer. “Evidence indicates that with increasing duration of exposure, progesterone can limit breast epithelial growth as it does with endometrial epithelium. Human breast tissue specimens removed after patients were treated with estradiol and progesterone indicate that progesterone inhibits in vivo estradiol-induced proliferation.” In the absence of progesterone, estrogen can induce excessive growth and proliferation of breast tissue. When produced in adequate amounts, estradiol promotes the production of growth factors responsible for progesterone receptor expression. If there is adequate progesterone receptor expression, progesterone can then slow the growth of breast tissue and promote better differentiation and estrogen receptor downregulation, resulting in greater inhibition of growth. Therefore, understanding the mechanisms of tissue-specific, normal growth regulation and the changes that occurred during the genesis of cancer may provide insights into both diagnostic and therapeutic importance.
There is epidemiological evidence for increased breast cancer incidence in women with a history of progesterone deficiency. Premenopausal women found to be progesterone-deficient had 5.4 times more premenopausal breast cancer than women with normal progesterone production. Interestingly, progesterone deficiency was also associated with 10 times the rate of death from all malignant neoplasms. Micheli found that the relative risk of breast cancer in premenopausal women was inversely associated with progesterone levels. These studies support the importance of adequate progesterone production during the luteal phase and the risk of breast cancer in premenopausal women. Since estrogen is directly responsible for progesterone production, this data underscores the importance of adequate estrogen levels in maintaining the health of the breast and the prevention of breast cancer.
A compelling area of research is being done on estrogen metabolites and their role in the treatment of breast cancer. An estrogen metabolite known as 2-methoxyestradiol (Panzem, an FDA-approved drug) is derived from estradiol and works by suppressing tumor growth and blocking the formation of new blood vessels that feed tumors. It has the ability to induce cancer cells to self-destruct through the process of apoptosis (programmed cell death) and to destroy blood vessels that feed tumors (anti-angiogenesis). In addition to treating sarcoma, lung, and brain cancers, 2-methoxyestradiol may be effective in treating breast cancer, particularly the spread of breast cancer.
Estrogen is Cancer-Protective
This data underscores the central role of estrogen in protecting the health of the breast and the need to understand estrogen’s role not only in the prevention but also in the treatment of breast cancer. Furthermore, logic dictates that the survival of the human species over millions of years implies that estradiol is not a health hazard to women. The hormones our bodies make (bio-identical), in both structure and function, have served women well for millions of years.
The fear of estrogen needs to end. And physicians need to educate themselves about the mental and physical benefits of it when it is fully restored, and what happens to a woman's brain and body when it remains deficient. And more importantly, trained on how to effectively and sustainably restore it in all their female patients, regardless of age.
.....
If it feels like your doctor is afraid of estrogen, or under the impression it causes cancer, your best bet is to find a hormone health team educated, trained, and experienced in full estrogen restoration. Who you go to for HRT help will make or break your hormone-balancing journey.
We are experts at helping women achieve and maintain optimal hormonal balance. Our advanced female hormone-balancing programs are not for everyone, but one could be just what you are looking for. Book a complimentary discovery session to see if working together is a good fit.
Reference:
Anderson G, Chlebowski R, Rossouw J, et al. (2006) Prior hormone therapy and breast cancer risk in the women’s health initiative randomized trial of estrogen plus progestin. Maturitas; 55:1-13.
Biglia N, Cozzarella M, Cacciari F, Ponzone R, et al. (2003) Menopause after breast cancer. Maturitas; 45:29-38.
Clarke C, Glaser S. (2007) Declines in breast cancer after the WHI: apparent impact of hormonal therapy. Cancer Causes Control; 18(8): 847-52
Cowan L, et al. (1981) Breast cancer incidence in women with a history of progesterone deficiency. American J Epidemiol; 114: 209-17.
Dixon BK. ‘Time to move forward’ for HRT. OB.GYN. News. 2006; 41(19):1-3.
Eure MA. 2005 Breast cancer risk increases with age. About.com.
HERS Sudy Report. HT can relieve menopausal-type symptoms common in elderly women. ACOG News Release 2002
Hays J, Ockene JK, Brenner RL, et al 2003 Effects of estrogen plus progestin on health-related quality of life. N Engl J Med. 348:1839-1854.
Jernstrom H, Bendahl P, Lidfeldt J, et al. (2003) A prospective study of different types of hormone replacement therapy use and the risk of subsequent breast cancer: The Women’s Health in the Lund Area (WHILA) study (Sweden). Cancer Causes Control; 97:1387-92
LaValle TM, et al. (2002) 2-methoxyestradiol inhibits proliferation and induces apoptosis independently of estrogen receptors α and β. Cancer Research; 62: 3691- 3697.
LaVallee TM, Zhan XH, Herbstritt CJ, Kough EC, Green SJ, Pribluda VS. 2Methoxyestradiol inhibits proliferation and induces apoptosis independently of estrogen receptor α and β. Cancer Research. 2002; 62:3691-3697.
Lewis-Wambi JS, Kim HR, Wambi C, Patel R, Pyle JR, Klein-Szanto AJ, Jordan VC. Buthionine sulfoximine sensitizes antihormone-resistant human breast cancer cells to estrogen-induced apoptosis. Breast Cancer Research. 2008; 10( 6).
Lewis JS, Meeke K, Ross EA, Kidawi N, Li T, Bell E, Chandel NS, Jordan VC. Intrinsic mechanisms of estradiol-induced apoptosis in breast cancer cells resistant to estrogen deprivation. J NatL Cancer Inst. 2005 Dec 7; 97(23):1746-1759.
Lewis-Wambi JS, Kim HR, Wambi C, Patel R, Pyle JR, Klein-Szanto AJ, Jordan VC. Buthionine sulfoximine sensitizes antihormone-resistant human breast cancer cells to estrogen-induced apoptosis. Breast Cancer Research. 2008; 10(6).
Lewis-Wambi JS, Jordan VC. Estrogen regulation of apoptosis: how can one hormone stimulates and inhibit? Breast Cancer Res. 2009; 11(3):206.
Lootta M, Escobar PF. (2011) Hormone replacement after breast cancer: Is it safe? Clinical Obstetrics and Gynecology; 54(1):173-179.
Micheli A, et al. (2004) Endogenous sex hormones and subsequent breast cancer in premenopausal women. Int J Cancer; 112: 312-318.
Naftolin F, et al 2004 The Women’s Health Initiative could not have detected cardioprotective effects of starting hormone therapy during the menopausal transition. Fertil Steri 81:1498-1501.
Newcomb PA, Egan KM, Trentham-Dietz A, Titus-Ernstoff L, et al. (2008) Pre-diagnostic use of hormone therapy and mortality after breast cancer. Cancer Epidemiol Biomarkers Prev; 17(4): 864-871.
O’Meara ES, Rossing MA, Daling JR, Elmore JG, Barlow WE, Weiss NS. (2001) Hormone replacement therapy after a diagnosis of breast cancer in relation to recurrence and mortality. J Natl Cancer Inst; 93(10):754-762.
Ross RK, Paganini-Hill A, Wan PC, Pike MC. 2000 Effect of hormone replacement therapy on breast cancer risk: Estrogen versus estrogen plus progestin. J Natl Cancer Inst; 92:328–32.
Salpeter, SR, Cheng J, Thabane L, Buckley NS, Salpeter EE. (2009) Bayesian meta-analysis of hormone therapy and mortality in younger postmenopausal women. Am J Med; 122(11): 1016-1022.
Science Daily Estrogen reduces breast cancer stem cells and aggression in breast cancer, study suggests. ( 2011, February 15) http://www.sciencedaily.com/releases/2011/02/110214083811.htm
http//seniorhealth.about.com/od/cancer/a/br_cancer_age.htmKelly, G. F. 1998 Sexuality Today: The Human Perspective. McGraw-Hill Companies.
Song RX, Santen RJ. Apoptotic action of estrogen. Apoptosis. 2003 Jan; 8(1):55-60.
Speroff L, Glass R, Kase N. Clinical Gynecologic Endocrinology and Fertility. 7th Edition, Lippincott Williamson Wilkins, Baltimore, MD, 2005, Pg. 599.
Turgeon JL, Carr MC, Maki PM, Mendelsohn ME, Wise PM. Complex actions of sex steroids in adipose tissue, the cardiovascular system, and brain: Insights from basic science and clinical studies. Endocrinology Reviews. 2006; 27(6):575-605
The Women's Health Initiative Steering Committee*. Effects of Conjugated Equine Estrogen in Postmenopausal Women With Hysterectomy: The Women's Health Initiative Randomized Controlled Trial. JAMA. 2004;291(14):1701–1712.
Xydakis AM, Sakkas EGR, Mastorakos G. (2006) Hormone replacement therapy in breast cancer survivors. Annals of the New York Academy of Sciences; 1092:349-360.
Join my mailing list to receive the latest news and updates on blog posts, new podcast episodes, in-person and online events, appearances, webinars, and programs.






